- Assessing hydration and nutrition status
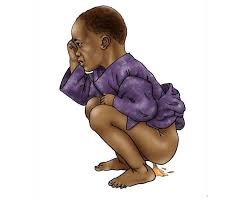
- Hydration status – An approach to assessment of hydration status based on four clinical signs has been issued by the World Health Organization (WHO)
- Temperature – Fever is common in the setting of diarrheal illness; however, the presence of fever or hypothermia should also prompt consideration of comorbid illnesses, such as pneumonia, sepsis, or malaria (in areas where endemic).
- Respiratory rate – Tachypnea may occur in patients with metabolic acidosis associated with dehydration, as well as in the setting of pneumonia.
- Abdomen – Presence of abdominal pain should prompt consideration for an additional intrabdominal process, such as obstruction, intussusception, or appendicitis.
- Central nervous system (CNS) – Moderate dehydration may be associated with irritability; severe dehydration can lead to lethargy and coma. Other manifestations of CNS involvement in the setting of diarrheal illness include seizures and encephalopathy.
Patients may present with bacterial meningitis and associated diarrhea; in infants with meningitis, meningeal signs may be absent.
- Eye exam – Patients should be examined for signs of vitamin A deficiency; these include corneal clouding and conjunctival lesions (Bitot spot) .
Investigations
The approach to diagnostic evaluation should be guided by clinical circumstances, as outlined below.
- Watery diarrhea – Stool microscopy and do culture to distinguish cholera from other causes of watery diarrhea.
A definitive diagnosis of cholera is established by stool culture; supportive diagnostic tools include darkfield microscopy for detection of motile vibrios (which appear as “shooting stars”) or a stool dipstick.
In the absence of diagnostic tools, patients with a short history (usually <24 hours) of vomiting and voluminous watery diarrhea with a characteristic rice-water appearance, especially in the setting of an outbreak, may be presumptively diagnosed with cholera based on clinical suspicion.
- Invasive (bloody) diarrhea – stool culture is warranted if feasible.
For patients who do not respond to antibiotic therapy, evaluation for E. histolytica is warranted via stool microscopy for the detection of trophozoites.
- Additional manifestations
- Fever – where malaria is endemic, malaria testing.
- Abdominal pain – For patients with watery diarrhea and abdominal pain who are not responsive to initial rehydration, imaging studies are warranted.
- Respiratory distress – For patients with respiratory distress, reassessment following initial rehydration is warranted. A chest radiograph is warranted for the evaluation of pneumonia, particularly in severely malnourished and dehydrated.
- Neurologic symptoms – For patients with neurologic symptoms, glucose and electrolyte assessments should be pursued.
